Presented by: Dimitrios Sakellaris, MD

Edited by: Penelope de Politis, MD
A 79-year-old woman presented with pain, redness and photophobia on the right eye.
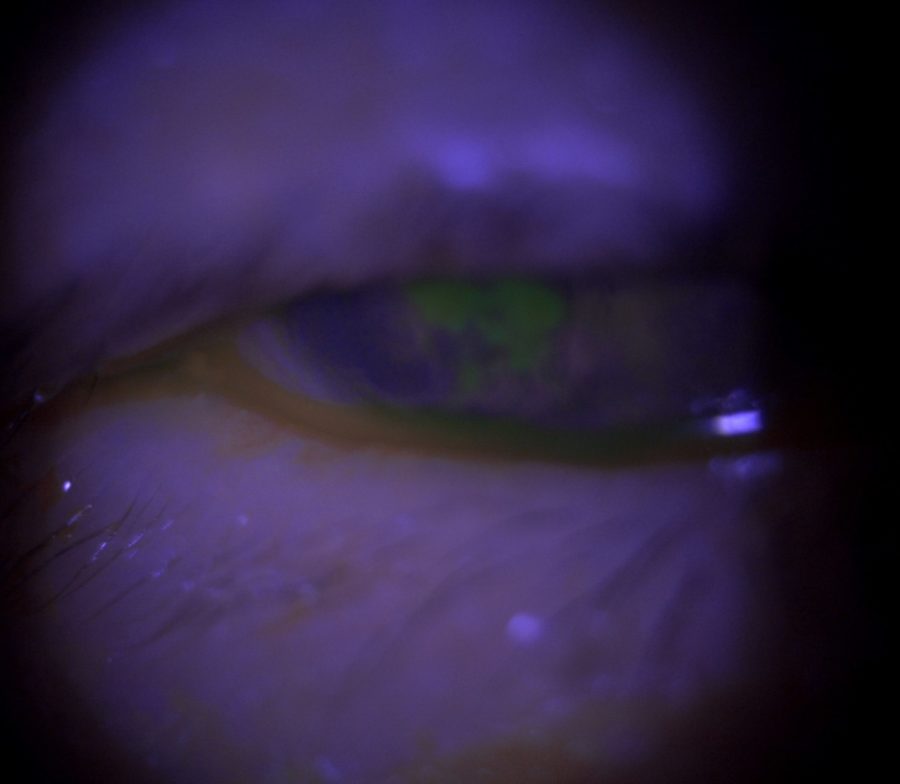
Figure 1: Microscope photograph under broad beam, blue filter direct illumination showing a paracentral corneal ulcer of approximately 3 X 4 mm, staining with fluorescein drops.
Case History
A 79-year-old Caucasian woman presented with pain, tearing, photophobia and redness on the right eye (RE) for a month, worsening in the last couple of days. The pain was intense, continuous, causing strong blepharospasm and requiring powerful analgesics. Upon emergency examination, a paracentral corneal ulcer of 3 X 4 mm was detected (Figure 1), with an adjacent area of corneal thinning and neovessels. Anterior chamber reaction was graded as 2+. There was mild lid edema and marked sensitivity to light. The left eye (LE) was slightly red but displayed no other signs of active inflammation. She was started on topical ceftazidime, moxifloxacin and vancomycin for the RE, with significant improvement noticed after 3 days.
Antibiotic medication was suspended once the lesion was fully epithelialized. However, neither eye was ever calm, bringing up suspicion for a chronic inflammatory ocular surface disorder, thus demanding further investigation and prolonged intervention. Long-term control was achieved with sparse administration of high-dose corticosteroid drops and lubrication on the RE and low-dose corticosteroid drops on the LE. Within the next few months, the patient underwent uneventful phacoemulsification for dense cataract on the RE, but vision remained low, due to age-related macular degeneration and corneal scarring (Figure 2). Best corrected distance visual acuity (BCDVA) achieved after surgery was finger count. BCDVA on the LE is now 6/10 and the patient is scheduled for cataract surgery on that eye.

Figure 2: Slit-lamp photograph showing a poorly demarcated area of corneal opacity, corresponding to the previous erosive lesion. Notice prominent adjacent neovessels.
Additional History
The patient had a long history of relapsing ocular inflammation, with little or no response to topical lubricants and mild corticosteroid drops. She had seen several ophthalmologists, but no additional exams had been requested yet. Symblepharon was evident on the RE (Figure 3), while on the LE there was merely a shallow lower fornix. Based on history and clinical findings, a suspicion for ocular cicatricial pemphigoid (OCP) was raised. A conjunctival biopsy was performed on the RE, rendering a negative result, defined as “chronic unspecified conjunctivitis”. A second biopsy was conducted, the sample sent to a different laboratory, this time with an affirmative histopathologic diagnosis of OCP.
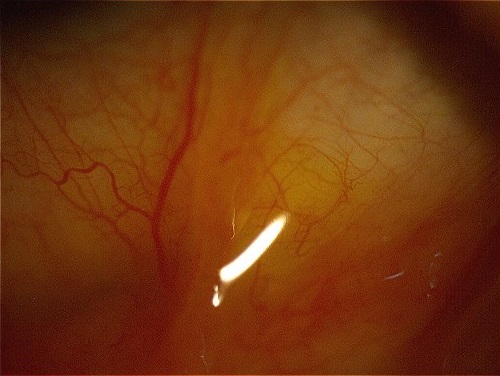
Figure 3: Direct-illumination photograph of the right lower fornice displaying an easily distinguishable, elevated symblepharon band.
Differential Diagnosis
- ocular cicatricial pemphigoid
- Stevens-Johnson syndrome
- dry eye syndrome
- history of adenoviral conjunctivitis
- atopic keratoconjunctivitis
- medicamentosa (from topical glaucoma and anti-herpetic medication)
- chemical burn
- trachoma
- radiation exposure
- toxic epidermal necrolysis
- graft-versus-host disease
- neoplasia
The differential diagnosis of OCP encompasses all forms of asymmetric bilateral chronic conjunctivitis with conjunctival scarring. A common confounder is medicamentosa, which induces pseudopemphigoid, a condition identical to OCP. A distinguishing feature is that symblephara of OCP are progressive. Definite distinction is made by conjunctival biopsies showing linear staining of the basement membrane.
Discussion and Literature
Ocular cicatricial pemphigoid (OCP) is a form of mucous membrane pemphigoid (MMP) presenting as a chronic, relapsing-remitting, bilateral conjunctivitis, leading to conjunctival scarring. A heterogeneous group of autoimmune subepithelial blistering disorders, MMP primarily affects orificial mucous membranes (conjunctiva, nasal cavity, trachea, mouth, oropharynx, esophagus, genitalia and anus), causing erosions, blisters and strictures. In some cases, there is also skin involvement.
Ocular cicatricial pemphigoid is present in 60% to 70% of patients with MMP. Considered a rare disease, with an estimated incidence of 1 per 10,000 to 50,000, OCP affects predominantly females (2:1 over males). The age of onset is around 60 years of age or older, though in studies age ranges from 20 to 91 years. There is no racial predilection. When unresponsive or left untreated, OCP progresses to ocular surface failure, inflammatory and infectious complications, corneal opacification and permanent vision loss.
The pathophysiological mechanism of OCP is a type 2 hypersensitivity reaction to the basal epithelial membrane of the conjunctiva. Like most autoimmune diseases, environmental factors and genetic susceptibility are believed to play a role in initiating a loss of tolerance to one or more components of the basal membrane zone (BMZ).
Conjunctival biopsy with direct immunofluorescence (DIF) is the most reliable method and the gold standard to confirm diagnosis, though 20% to 40% of patients with clinically evident OCP may have a negative biopsy. When positive, there is a linear antibody deposition in the epithelial BMZ. Histological analysis can help differentiate from neoplasia if DIF is inconclusive. Hematoxylin-eosin (H&E) often displays an inflammatory stain pattern. Periodic acid–Schiff (PAS) stains show a decrease in goblet cells, while in Giemsa stains there is an increased mast cell population.
Management of OCP is aimed at controlling the immune-mediated inflammatory disease, preventing fibrosis, and managing ocular surface disruption. Early diagnosis and appropriate treatment are of paramount importance and require a high level of expertise as the condition can be extremely challenging, even for experienced specialists. Systemic immunosuppression is sometimes required to control inflammatory reaction and halt fibrosis, preventing progression to more advanced stages. Topical treatment is useful for managing surface inflammation and providing symptomatic relief.
Keep in mind
- OCP is a challenging surface disorder, both to diagnose and to treat.
- A thorough history and careful slit-lamp examination must be added to conjunctival biopsy for precise diagnosis. A second biopsy may be needed when history and ocular findings point to OCP and a first sample comes out negative.
- Management of OCP requires prompt and attentive intervention, in order to prevent surface scarring, severe lid changes and loss of vision.
References
- Schonberg S & Stokkermans TJ. Ocular Pemphigoid. [Updated 2021 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526100/
- Tolaymat L & Hall MR. Cicatricial Pemphigoid. [Updated 2020 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526120/
- Vazirani J, Donthineni PR, Goel S, Sane SS, Mahuvakar S, Narang P, Shanbhag SS & Basu S. (2020). Chronic cicatrizing conjunctivitis: A review of the differential diagnosis and an algorithmic approach to management. Indian journal of ophthalmology, 68(11), 2349–2355. https://doi.org/10.4103/ijo.IJO_604_20
- Branisteanu DC, Stoleriu G, Branisteanu DE, Boda D, Branisteanu CI, Maranduca MA, Moraru A, Stanca HT, Zemba M & Balta F. (2020). Ocular cicatricial pemphigoid (Review). Experimental and therapeutic medicine, 20(4), 3379–3382. https://doi.org/10.3892/etm.2020.8972
- Stan C, Diaconu E, Hopirca L, Petra N, Rednic A & Stan C. (2020). Ocular cicatricial pemphigoid. Romanian journal of ophthalmology, 64(2), 226–230. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7339695/
- Georgoudis P, Sabatino F, Szentmary N, Palioura S, Fodor E, Hamada S, Scholl H & Gatzioufas Z. (2019). Ocular Mucous Membrane Pemphigoid: Current State of Pathophysiology, Diagnostics and Treatment. Ophthalmology and therapy, 8(1), 5–17. https://doi.org/10.1007/s40123-019-0164-z
- https://eyewiki.aao.org/Ocular_Cicatricial_Pemphigoid

