Presented by: Paris Tranos MD, PhD, ICOphth, FRCS

Edited by: Penelope Burle de Politis, MD

An 11-year-old boy presented with an acute paracentral scotoma in his right eye.
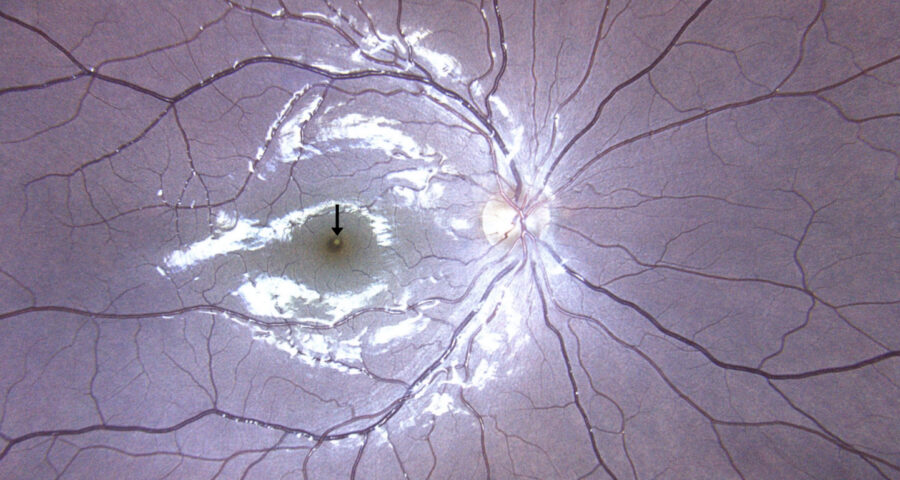
Figure 1: Color fundus photograph (EIDON true-color confocal scanner®) displaying a focal yellowish discoloration at the right fovea (black arrow).
Case History
An 11-year-old Caucasian boy presented with a paracentral scotoma in the right eye (RE) that he had noticed the day before his visit. He was previously healthy, and his ocular history was unremarkable. There was no relevant family history. Upon examination, his visual acuity was 10/10 in both eyes. Intraocular pressure was within normal limits bilaterally, and anterior segment biomicroscopy showed no abnormalities. Fundoscopy was unremarkable on the left eye but revealed a focal yellow-white discoloration at the fovea on the right (Figure 1). Amsler grid testing detected a small paracentral inferior distortion in the RE, in correspondence with the foveal lesion.
Spectral domain optical coherence tomography (SD-OCT) identified a characteristic “ASHH sign” (angular sign of Henle’s fiber layer hyperreflectivity) at the right fovea (Figure 2).
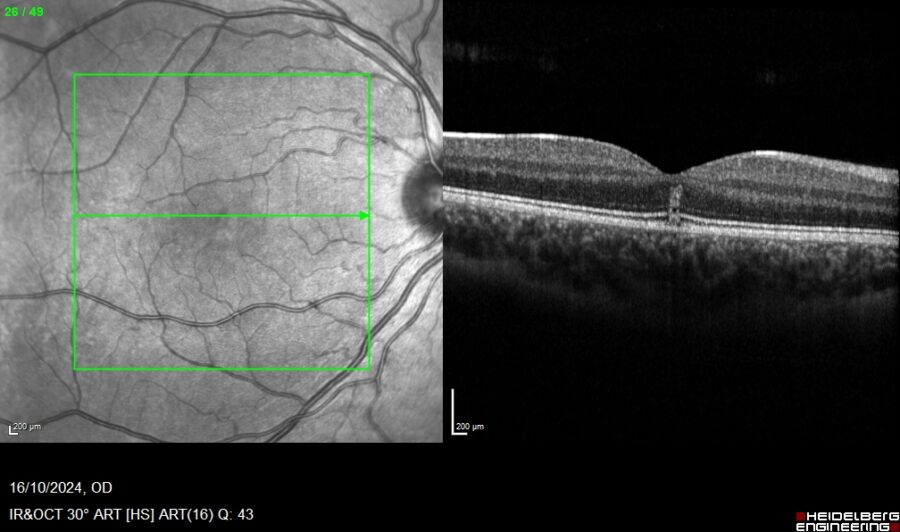
Figure 2: SD-OCT (Heidelberg Engineering®) of the right eye illustrating a hyperreflective lesion invading the Henle’s fiber layer (ASHH sign), along with focal disruption of the ellipsoid zone.
Blue-light fundus autofluorescence (BAF) was normal in BE, while a focal defect on the choriocapillaris was noted on the OCT-angiogram (Figure 3).
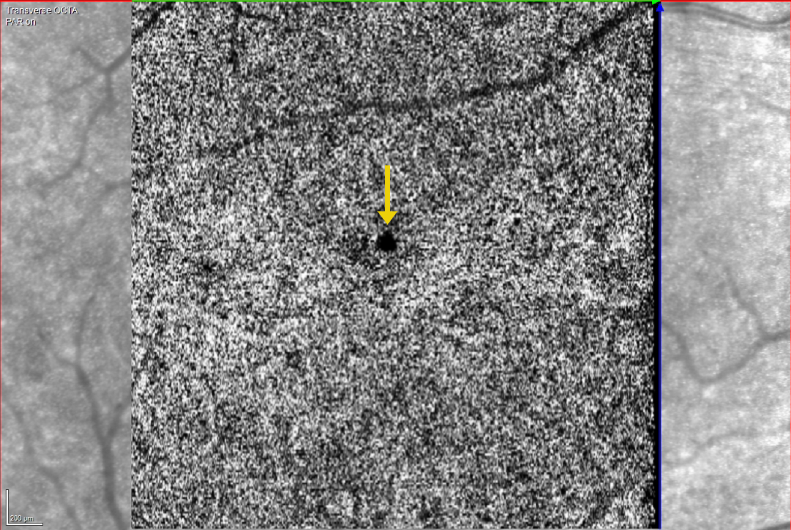
Figure 3: OCT-angiogram (OCT-A, Heidelberg Engineering®) of the right eye demonstrating a focal defect at the level of the choriocapillaris (yellow arrow).
Additional History
The patient reported that a green-laser beam had been accidentally pointed at his RE the day before his symptoms began. Based on the history of laser exposure and multimodal imaging findings, the diagnosis of handheld laser-induced maculopathy (HLIM) was established.
At the one-month review examination, visual acuity remained stable, and the visual field defect had improved. OCT imaging showed resolution of the foveal lesion (Figure 4), and the OCT-A displayed reduction of the choroidal flow void area.
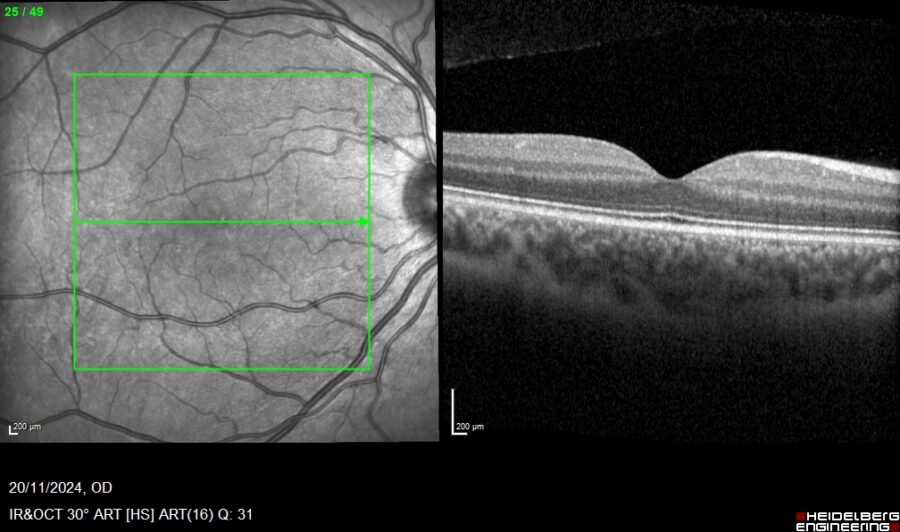
Figure 4: SD-OCT (Heidelberg Engineering®) of the right eye depicting resolution of the foveal lesion at 1-month follow-up.
Differential Diagnosis of Handheld Laser-Induced Maculopathy
- solar retinopathy
- phototoxic retinopathy
- macular inflammatory conditions (punctate inner choroidopathy, acute posterior multifocal placoid pigment epitheliopathy etc.)
- macular microhole
Laser pointer retinopathy should be considered in cases of sudden-onset, painless vision loss, especially in children. The differential diagnosis of HLIM relies on obtaining a detailed history and identifying specific imaging characteristics. Handheld laser pointers cause direct photothermal injury to the retinal pigment epithelium and inner choroid, with corresponding disruption of the photoreceptor layer evident on SD-OCT.
Discussion and Literature
Laser pointers have become easily available as tools and toys. However, the risks of handling these devices are often underestimated. Children, in particular, are at risk of irreversible injury to themselves and others through irresponsible use of incorrectly labeled laser pointers. Laser pointer-induced retinopathy is increasingly common due to unrestricted online sales of high-power laser devices.
Laser light can cause retinal lesions in 3 manners: photomechanical, thermal and photochemical. Lasers are classified according to their accessible emission limits (AEL) by the IEC (International Electrotechnical Commission) and have power ratings from 1 to 4. Exposure to class 3 and 4 lasers (> 1 mW) is potentially harmful to the eye. In addition to power rate, light wavelength and color play an important role as green is more easily absorbed and therefore causes more damage to the retina compared to red.
The Food and Drug Administration (FDA) has identified 4 major classes of lasers, laser pointers belonging to class 3R. Exposure to direct or even reflected beams should be avoided without eye protection for class 3 or 4 lasers. Injuries to the eye can occur within moments of exposure to class 3 lasers, and protective mechanisms such as blinking or looking away are ineffective with such high powers.
Even when low-power lasers are used, photothermal injury to the retina may occur with prolonged exposure. While all ocular compartments can be damaged by lasers, the retina is peculiarly vulnerable. The human lens focuses the laser farther into the retina, which increases the power of the laser. The self-inflicted lesions affecting mainly the central and the superior part of the macula are related to Bell’s phenomenon.
The average age of patients with macular injuries from recreational laser use has dropped exponentially, young males being most frequently affected. Children are at a greater risk than adults as they are intrigued by the laser appearance and have clearer ocular media and less effective protective mechanisms like blinking and gaze aversion than adults. Children with mental health, behavioural or learning issues are even more susceptible to accidental laser-pointer ocular exposure.
Symptoms of laser pointer-induced retinopathy include loss of visual acuity, central or paracentral scotomas, metamorphopsia, and dyschromatopsia. Retinal damage can manifest as subretinal or intraretinal hemorrhage, retinal edema, macular streaks, retinal pigment epithelium scarring, foveal granularity, vitreous or chorioretinal hemorrhage, perifoveal drusenoid deposits, ring-shaped hypopigmented foveal lesions, macular holes, or, rarely, choroidal neovascularization.
Diagnosing laser pointer-induced retinopathy is challenging, as children may not report or deny exposure, and retinal findings are not pathognomonic. Early signs on multimodal imaging and careful history-taking are crucial. Retinal damage by laser pointers is subject to dynamic changes, especially in the first weeks after the onset of injury. Although some lesions resolve spontaneously if Bruch’s membrane remains intact, permanent structural damage and complications like secondary choroidal neovascularization may develop over time.
Therapeutic options are limited, with corticosteroids occasionally used, though their benefit is debatable. Both preclinical and clinical data are difficult to interpret due to the favorable natural course of the disease in most cases. Since most incidents are preventable, the focus should be on increasing public awareness and enforcing regulations to limit the availability of high-power laser devices.
Keep in mind
- Handheld laser-induced maculopathy is on the rise due to increasingly indiscriminate access to laser pointer devices.
- Laser pointer-induced retinopathy must be suspected whenever there is sudden-onset, painless vision loss, especially in children.
- Even though laser pointer-induced macular injury usually has a benign course, there may be permanent structural damage to the retina.
References
- Gregori NZ, Cai L & Moshiri Y (2024). Self-Inflicted Laser-Induced Retinopathy. Diagnostics (Basel, Switzerland), 14(4), 361. https://doi.org/10.3390/diagnostics14040361
- Farassat N, Boehringer D, Luebke J, Ness T, Agostini H, Reinhard T, Lagrèze WA & Reich M (2023). Incidence and long-term outcome of laser pointer maculopathy in children. International ophthalmology, 43(7), 2397–2405. https://doi.org/10.1007/s10792-023-02638-w
- Chen Y, Cunningham A & Kotagiri A (2023). The Danger of Laser Pointer-Induced Retinal Damage in Children: A Large United Kingdom Case Series and Survey of Public Awareness. Journal of pediatric ophthalmology and strabismus, 60(1), 52–59. https://doi.org/10.3928/01913913-20220425-01
- Al Adel F & AlBloushi AF (2021). Laser-Induced Maculopathy Masquerading as Hereditary Macular Dystrophy. Middle East African journal of ophthalmology, 28(3), 189–192. https://doi.org/10.4103/meajo.meajo_234_21
- Narayanan R, Tyagi M, Sahoo NK, Reddy S & Pathengay A (2023). Accidental Self-Inflicted Handheld Laser-Induced Maculopathy. Ocular immunology and inflammation, 31(1), 211–214. https://doi.org/10.1080/09273948.2021.1988987
- Mehta N, Tsui E, Ranka M, Dedania V, Lee GD & Modi Y (2018). Inadvertent self-induced macular laser injury in an 8-year-old girl. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus, 22(5), 397–398. https://www.jaapos.org/article/S1091-8531(18)30114-9/abstract
- Linton E, Walkden A, Steeples LR et al. Retinal burns from laser pointers: a risk in children with behavioural problems. Eye 33, 492–504 (2019). https://doi.org/10.1038/s41433-018-0276-z
- Torp-Pedersen T, Welinder L, Justesen B, Christensen UC, Solborg Bjerrum S, La Cour M & Saunte JP (2018). Laser pointer maculopathy – on the rise?. Acta ophthalmologica, 96(7), 749–754. https://doi.org/10.1111/aos.13856
- Clemente-Tomás R, Bayo-Calduch P, Neira-Ibáñez P, Gargallo-Benedicto A & Duch-Samper AM (2018). Bilateral maculopathy after exposure to a laser pointer: Optical coherence tomography angiography findings. Maculopatía bilateral por exposición a puntero láser: hallazgos en la angiografía mediante tomografía de coherencia óptica. Archivos de la Sociedad Espanola de Oftalmologia, 93(11), 551–554. https://doi.org/10.1016/j.oftal.2017.12.020
- Ortiz Salvador M, Montero Hernández J, Castro Navarro V, Cervera Taulet E, Navarro Palop C, Monferrer Adsuara C, Remolí Sargues L & Gonzalez Girón N (2021). Multimodal imaging in phototoxic maculopathy: description of findings in a series of 12 patients. Imagen multimodal en la maculopatía fototóxica: descripción de hallazgos en una serie de 12 pacientes. Archivos de la Sociedad Espanola de Oftalmologia, 96(3), 133–140. https://doi.org/10.1016/j.oftal.2020.07.029

